Oral Presentation International Association of the Diabetes and Pregnancy Study Groups 2022 - Hosted by ADIPS
Trends in outcomes of pregnancies complicated by diabetes among First Nations and non-First Nations women in the Northern Territory, Australia (#34)
Background:
GDM and pre-existing diabetes in pregnancy (pre-existing DM) increase risk of obstetric and neonatal complications. In the Northern Territory (NT) of Australia, pregnant First Nations women have among the highest rates of pre-existing DM globally, with a 10-fold increase over the last 30 years.
Aim:
To gain contemporary risk estimates for and examine trends in obstetric and neonatal outcomes of GDM and pre-existing DM among pregnant First Nations and non-First Nations women in the NT.
Methods:
This retrospective population-based cohort study examined linked deidentified data from the NT Perinatal Data Collection and Hospital Inpatient Activity data relating to all births in the NT from 2002-2016. Poisson regression was used to assess relative risk and temporal trends by diabetes status in pregnancy separately among First Nations and non-First Nations women. Models were adjusted for maternal age, parity, remoteness and smoking.
Results:
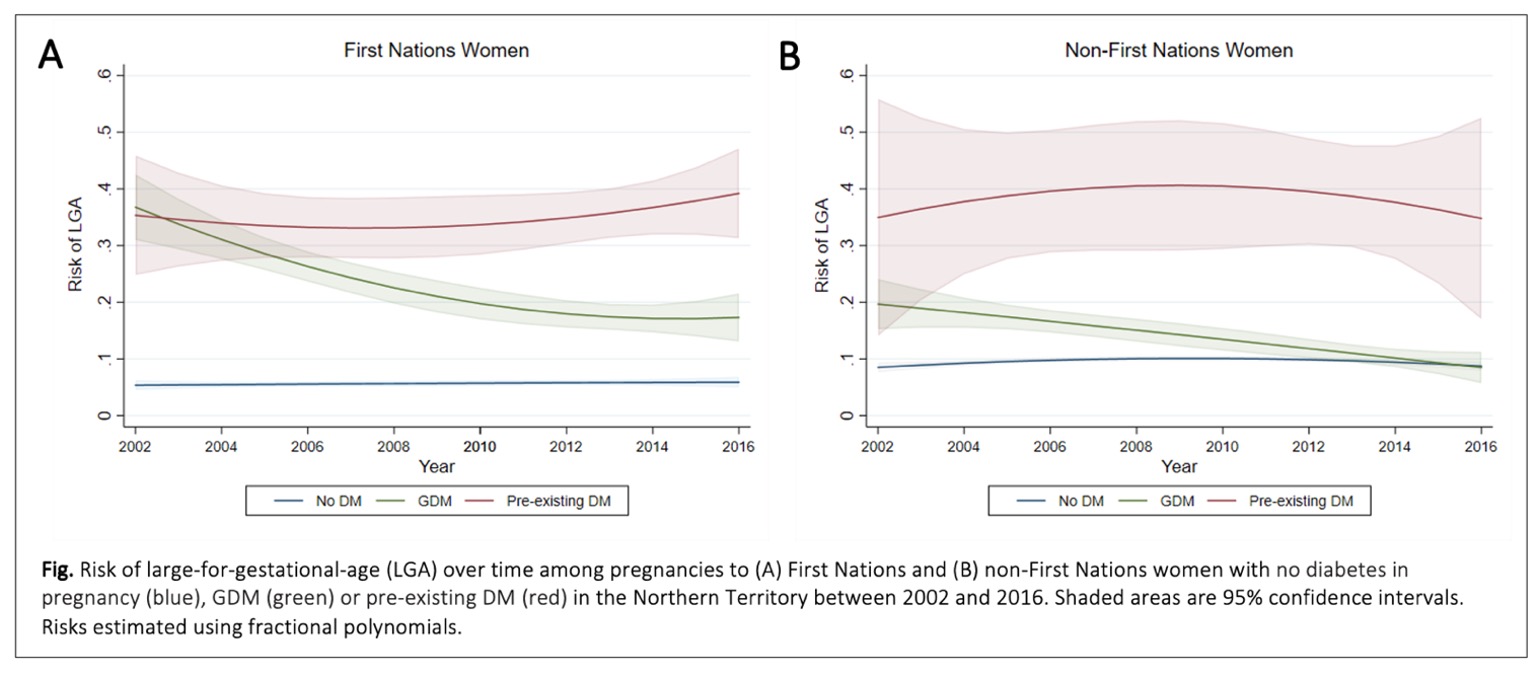
Of 57,707 pregnancies 21,061 (37%) were in First Nations women. Rates of GDM and pre-existing DM were 9.6% and 3.4% respectively, among First Nations women; and 5.5% and 0.5% among non-First Nations women, respectively. Risk of large-for-gestational-age (LGA) declined among both First Nations women with GDM (-5.3% per annum (p.a), p<0.001) and non-First Nations women with GDM (-5.5% p.a., p<0.001), but remained unchanged for women with pre-existing DM (see Fig.). Preeclampsia risk declined among both First Nations women with GDM (-7.2% p.a., p<0.001) and non-First Nations women with GDM (-4.7% p.a., p=0.010), but remained stable for women with pre-existing DM. Risk of emergency Caesarean section declined for First Nations women with GDM (-3.3% p.a., p=0.001), but remained stable for all other groups. Risk of preterm birth remained unchanged over time for all groups.
Conclusion:
Over 15 years, risk of LGA and preeclampsia reduced substantially for women with GDM, which may reflect improvement in management and changes in screening. Risk of adverse pregnancy outcomes remains high among all women with pre-existing DM, necessitating work to strengthen models of care.